Intervention 5
Aortic Stenosis: From Percutaneous Aortic Valve Implantation to Future Prevention Scenarios

Ciro Indolfi, MD, PhD
Magna Graecia University, Italy
It is well known that the natural history of aortic stenosis has changed significantly today (red in figure) compared to the original description by Dr. J. Ross Jr. in patients with rheumatic aortic stenosis. In particular, the onset of symptoms in degenerative-calcific aortic stenosis dramatically alters the natural progression of the disease, with a survival rate of only 2 years for those presenting with heart failure (see figure). The mechanisms behind degenerative aortic stenosis are still only partially understood, with links to inflammation, elevated Lp(a) levels, and even amyloidosis.
We can state that, following the introduction of coronary stents, transcatheter aortic valve implantation (TAVI) is the most significant innovation in interventional cardiology. TAVI is now a standard of care and is expected to become the preferred therapeutic strategy for most cases of aortic stenosis requiring biological valve implantation.
In 2023, 91 TAVI procedures per million inhabitants were performed in Europe.
From a clinical standpoint, several randomized studies have shown that TAVI is superior to medical therapy and outperforms surgery in high-risk patients. In low-risk patients, TAVI is either comparable to or even better than surgery.
The superiority of TAVI over surgery has been demonstrated, particularly when the femoral artery approach is used. However, issues related to durability, coronary artery access, and the need for pacemaker implantation still require further study in low-risk patients.
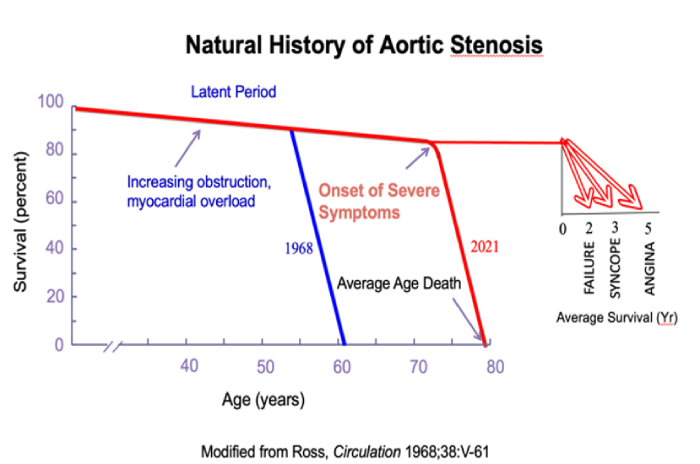
Figure 1. Natural history of patients with aortic stenosis