Hypertension 2
Use of Cuffless BP Device in the Clinical Setting: Can It Replace ABPM?

Hae-Young Lee, MD, PhD
Seoul National University, KoreaHypertension management is undergoing a transformative shift towards comprehensive 24-hour blood pressure (BP) control, including nighttime monitoring. Recent global hypertension guidelines emphasize the importance of home BP monitoring and 24-hour ambulatory BP measurement for accurate diagnoses and treatment plans. However, the patient’s discomfort during ambulatory BP measurement and the technical issue in automatic measurement in nighttime in case of home BP monitoring limit widespread adoption. Despite these challenges, integrating BP measurement into mobile devices offers a promising avenue for monitoring BP outside clinical settings. Innovations include smartwatches utilizing photoplethysmography (PPG) sensors and machine learning algorithms. Although promising, these devices face concerns regarding accuracy and the need for periodic calibration. And other challenges such as verifying device accuracy, interpreting vast amounts of data, and ensuring reliable calibration need to be addressed.(Figure 1)
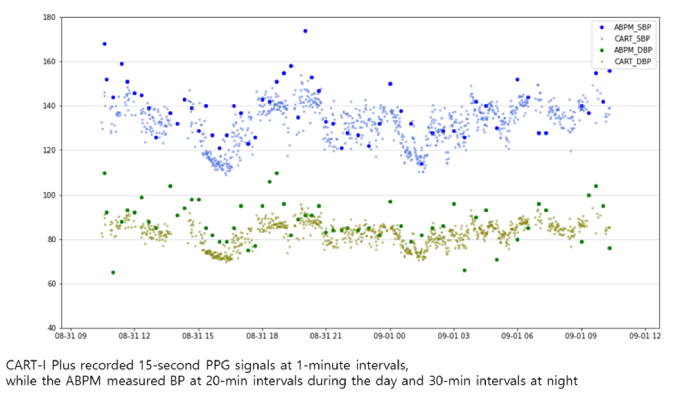
Figure 1. CART-I Plus recorded 15-second PPG signals at 1-minute intervals, While the ABPM measured BP at 20-min intervals during the day and 30-min intervals at night
Despite all these current limitation, mobile device BP monitoring represents a significant advancement in hypertension management, offering the potential for continuous, convenient, and less intrusive BP monitoring. The integration of BP measurements using smartwatches and other wearables might open a new field of dynamic evaluation of BP. Conventional BP measurement methods, including ABPM, mainly focus on static BP measurements in a resting state. However, wearable technology allows for the continuous monitoring of BP changes in daily living and during physical or emotional stress. This dynamic BP monitoring could provide a more comprehensive understanding of BP patterns and their impact on cardiovascular health.
In conclusion, mobile device BP monitoring holds the potential to revolutionize hypertension management. Despite the potential benefits, challenges such as verifying device accuracy, interpreting data, and ensuring calibration need to be addressed. The future of hypertension management will likely rely on these technologies, alongside traditional methods, to offer a more comprehensive understanding of an individual's BP profile. This integration promises to improve hypertension diagnosis, management, and patient outcomes, though further research and development are necessary to overcome current limitations. Innovations in wearable BP monitoring technology offer exciting possibilities for more personalized and effective hypertension care. As these technologies evolve, they will likely play a crucial role in reducing the burden of hypertension-related cardiovascular diseases and improving patient outcomes globally.