Arrhythmia
Roles of Programed electrical Stimulation Test in Channelopathies
Namsik Yoon, MD, PhD
Chonnam National University, Korea
There have been many reports studied the role of electrophysiologic study (EPS) in Brugada syndrome (BrS). In this presentation, the audience would
have a chance to review evidences of current recommendation.
In 2003, high sudden cardiac death (SCD) probability (HR 5.88) was identified in patients with BrS who develop ventricular fibrillation (VF) in EPS.
Brugada et al reported implantable cardioverter-defibrillator (ICD) may be considered in asymptomatic patients with spontaneous type 1 BrS ECG
and a family history in whom EPS is positive (IIa). They also reported ICD may be considered in asymptomatic patients with induced type 1 BrS
ECG (IIa) and family history in whom EPS is positive (IIb). However, FINGER and PRELUDE study showed no difference of arrhythmia-free survival
between VF inducible/non-inducible.
In terms of guidelines, HRS/EHRA/APHRS Expert Consensus 2013 documented ICD may be considered in BrS who develop VF during programmed electrical
stimulation (PES, IIb). ESC 2015 said ICD may be considered in patients with a diagnosis of BrS who develop VF during PES with two or three
ventricular extrastimuli at two sites (IIb, C). J-W syndromes experts consensus (2016) reported ICD may be considered in patients with asymptomatic
fever-induced type 1 BrS pattern ECG in whom inducible VF with upto 2 extrastimuli. AHA/ACC/HRA 2017 documented EPS may be considered for risk
stratification in spontaneous BrS ECG pattern without symptom. APHRS/HRS 2020, EPS may be considered in SCD survivor with no other disorder. Lastly,
European Society of Cardiology (ESC) 2022 described PES may be considered in asymptomatic patients with a spontaneous type I BrS ECG for risk stratification
(IIb, B), ICD implantation may be considered in selected asymptomatic BrS patients with inducible VF during PES using up to 2 extra stimuli (IIb, C).
On the other hand, Bhonsale et al showed event-free survival benefit in patients with arrhythmogenic right ventricular cardiomyopathy (ARVC) who
shows non-inducible at EPS. AHA/ACC/HRS 2017 reported EPS is not recommended for risk stratification for ventricular arrhythmia (VA) in long QT
syndrome (LQTS), catecholaminergic polymorphic ventricular tachycardia (CPVT), short QT syndrome, or early repolarization syndrome. APHRS/HRS
2020 described electroanatomic mapping of right ventricle may be considered for detection of subclinical arrhythmogenic cardiomyopathy in SCD
survivors with no other disorder. Lastly, ESC 2022 reported detailed electroanatomic mapping may also reveal localized structural alterations
in idiopathic VF and PES is not recommended for stratification of SCD risk in LQTS, CPVT, short QT syndrome (III).
According to current guidelines, there is no need of EPS for BrS diagnosis in spontaneous type I BrS ECG because the ECG is enough to diagnose BrS.
However, for risk stratification, the question has not been answered completely. Our group reported no difference of ICD shock between inducible
VF and non-inducible (Figure). Further study would answer the question.
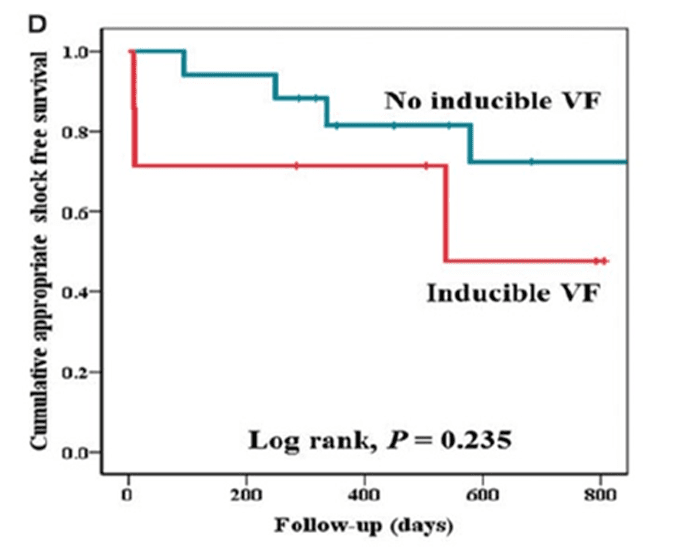
Figure 1. The initial ventricular fibrillation (VF) inducibility was not related with ventricular arrhythmia (EP Europace 2017)