Intervention
Preventive PCI for Functionally Insignificant Vulnerable Plaque: PREVENT Trial

Jung-Min Ahn, MD, PhD
Ulsan University., Korea
Acute coronary syndrome, often presenting as sudden cardiac deaths is commonly caused by the rupture of lipid-rich vulnerable
plaques in the coronary arteries, even in the absence of significant flow limitation. While standard pharmacologic treatments including
statin therapy are widely used to stabilize these vulnerable plaques and improve patient outcomes, the local treatment of preventive
percutaneous coronary intervention (PCI) for these vulnerable plaques has not been clearly established in terms of safety and efficacy.
Thus, the PREVENT study, a multinational, multicenter randomized trial, was conducted to evaluate the clinical effect of preventive PCI for these plaques.
From September 2015 through September 2021, enrollment was conducted across 15 research hospitals in South Korea, Japan, Taiwan, and New
Zealand. A total of 5,627 patients were screened for eligibility, and 1,606 patients were enrolled in the study. Participants had significant
coronary lesions (diameter stenosis >50% by angiographic assessment) without significant flow limitation assessed by Fractional Flow Reserve
(≥0.80), which were evaluated by intravascular imaging. Vulnerable plaques were defined as having a minimal lumen area of less than 4.0 mm²,
a plaque burden of 70% or more, lipid core burden index of 315 or more, or as thin-cap fibroatheroma
Participants were randomly assigned in a 1:1 ratio to either the preventive PCI group (803 patients) or the optimal medical therapy (OMT)
group (803 patients). In the preventive PCI group, bioabsorbable vascular scaffolds (BVS) were initially used, later replaced by
everolimus-eluting stents (Xience stents). Both groups underwent rigorous management of cardiovascular risk factors, with an average
LDL level of 64 mg/dL.
The primary endpoint was defined as a composite of cardiac death, target vessel myocardial infarction, target vessel revascularization,
and hospitalization for a composite clinical event at 2 years after randomization. The incidence of the primary outcome was significantly
lower in the preventive PCI group (0.4%, 3 patients) compared to the OMT group (3.4%, 27 patients), and this clinical benefit of preventive
PCI was maintained throughout the 7-year follow-up period. Additionally, a clinical equipoise was achieved across all major components
of the primary outcome in the preventive PCI group(Figure 1). Adverse events related to preventive PCI procedures were rare.
The results of this study represent the first large-scale randomized controlled trial demonstrating that preventive PCI can improve
clinical outcomes in patients with vulnerable plaques. It highlights the importance of considering the characteristics of
vulnerable plaques, along with clinical presentation and FFR, in the management of coronary artery disease, and suggests that
preventive PCI could be a viable alternative. This study may serve as an important milestone for future research and the development
of clinical guidelines concerning vulnerable plaques. However, additional clinical research and analysis will be needed to apply these
results to routine clinical practice.
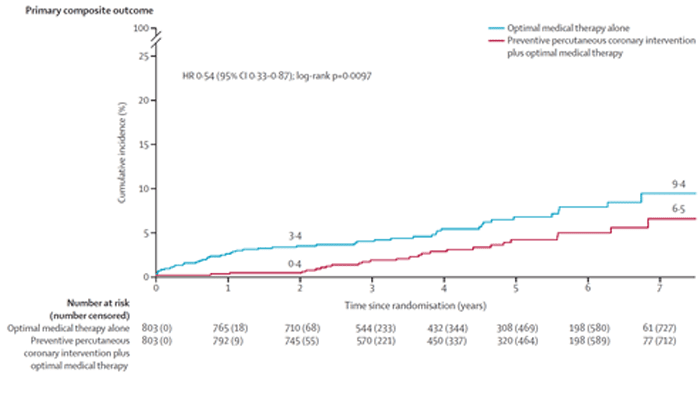
Figure 1. Time-to-event curves for the primary composite outcome