JCS-KSC Joint Session
Impact of Tissue Proximity Indication on Pulmonary Vein Isolation Success Using Pulsed Field Ablation with the VARIPULSE® Catheter: Insights from a Porcine Study and Initial Clinical Experience

Yasuo Okumura, MD, PhD
Nihon University, Japan
Pulsed field ablation (PFA) for paroxysmal atrial fibrillation (PAF) is gaining acceptance for its efficacy and safety. The VARIPULSE® circular catheter, recently launched in Japan, includes a Tissue Proximity Indication (TPI) feature to monitor catheter-tissue contact. The impact of TPI on lesion formation, however, remains unclear.
In five porcine models, PFA was applied at 35 atrial sites using the VARIPULSE® catheter with CARTO 3™. Lesions were compared between no/minimum contact (TPI-negative/flickering) and consistent contact (TPI-positive), confirmed by ultrasound. In 11 PAF patients, we assessed the relationship between TPI-positive sites, voltage, PV wall thickness, and PV isolation failure.
Lesions were significantly larger (lesion length: 36.0±12.5 mm vs. 17.4±15.2 mm; P=0.003; maximum width: 10.3±2.7 mm vs. 5.7±5.1 mm; P=0.009) and more transmural with consistent contact as compared to no/minimum contact (100% vs. 54.5%; P<0.001). In patients, two experienced 5 PV isolation failure sites, associated with lower TPI-positive percentages (0±12% vs. 64±1%, P<0.001) and higher voltage (2.93±0.47 mV vs. 1.69±0.06 mV, P=0.009) (figure). Failure occurred early in the learning curve, with TPI-positive percentages improving over time (42±4% to 75±4%, P<0.001).
Consistent TPI-based contact during PFA is strongly linked to distinct transmural lesion formation. Acute PVI failure was significantly associated with poor tissue contact and higher voltage. These findings highlight the importance of ensuring proper tissue contact for optimal outcomes with circular PFA catheters.
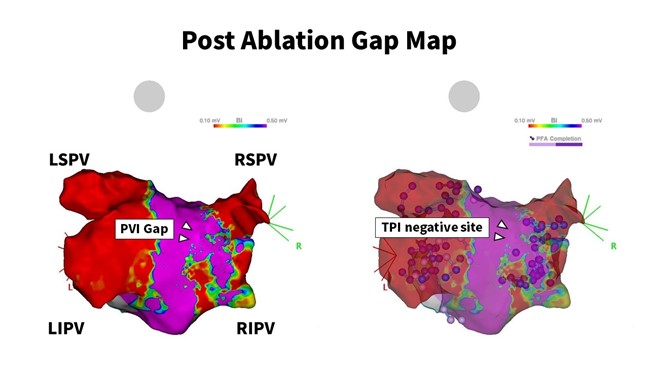
Figure